What is Frozen Shoulder?
Frozen shoulder, also known as adhesive capsulitis, is a condition that affects the shoulder joint, causing stiffness and pain. It can significantly hinder daily activities and limit the range of motion. Understanding its causes and symptoms is essential for those who may be suffering from this ailment.
If you’ve been struggling with shoulder stiffness or limited motion, understanding frozen shoulder causes and symptoms is the first step toward recovery. This common condition can affect anyone, especially middle-aged adults, leading to pain, discomfort, and restricted movement.
Causes of Frozen Shoulder
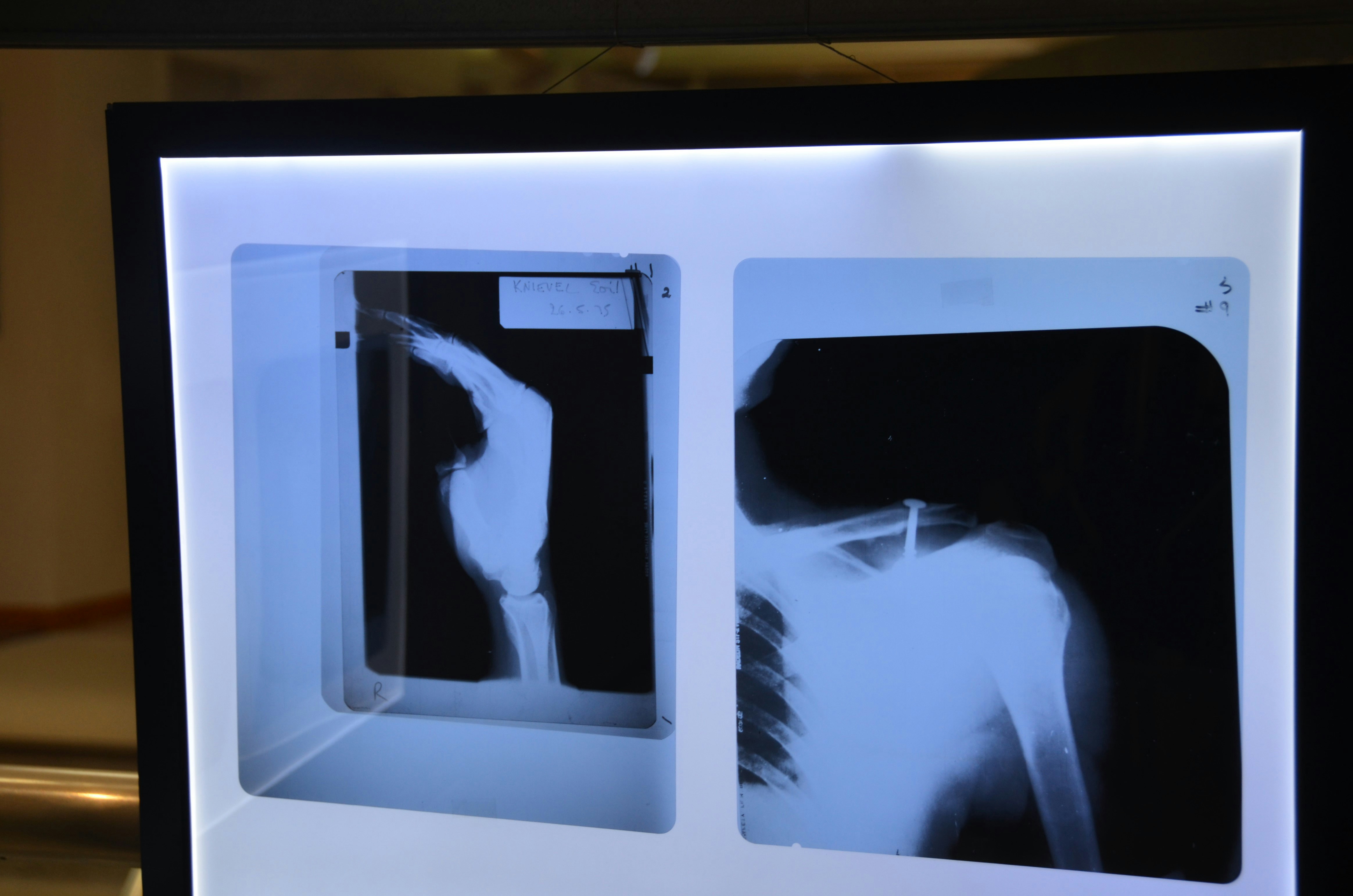
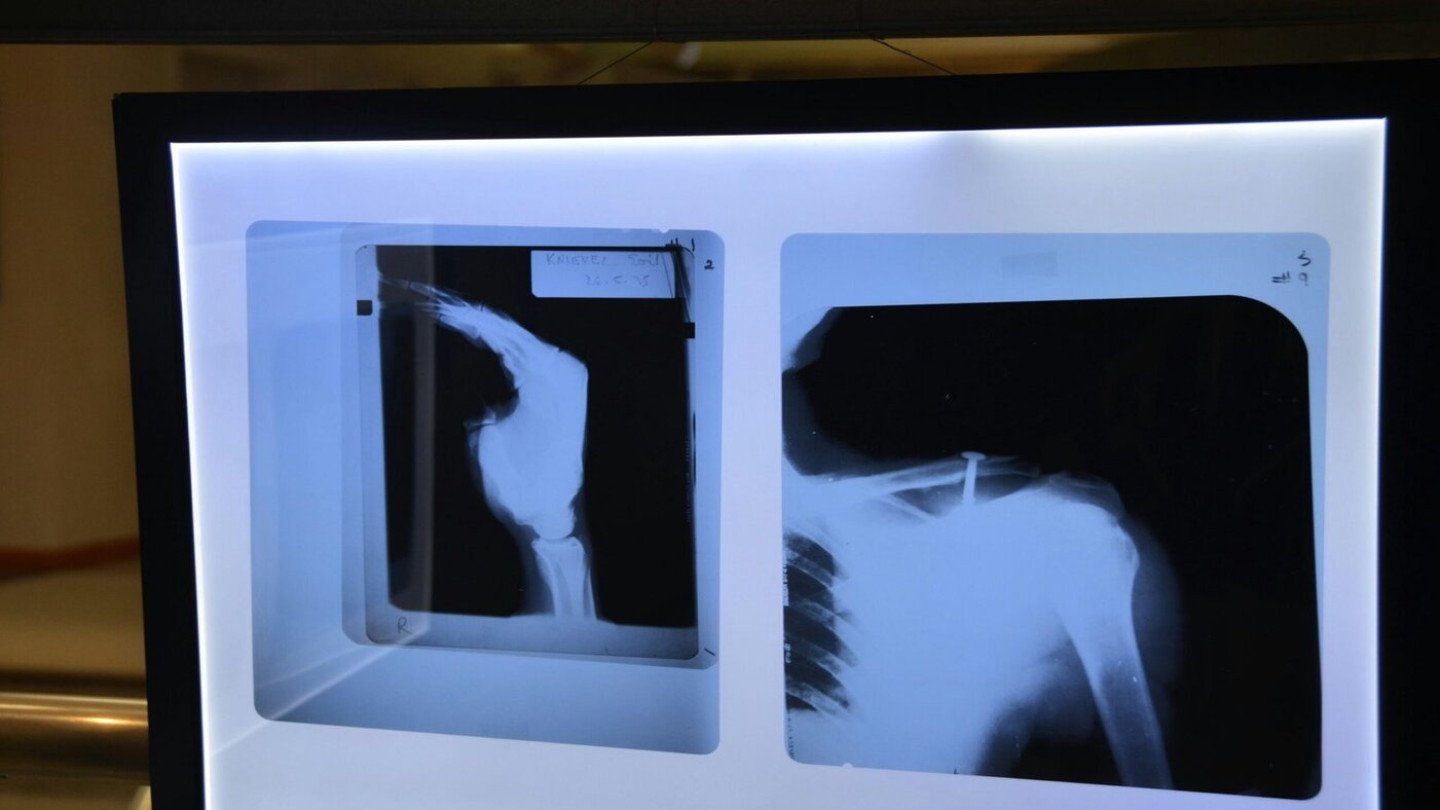
The exact cause of frozen shoulder is not entirely clear; however, certain factors are known to increase the risk. People who have diabetes, thyroid disorders, or those who have experienced shoulder injuries may be more susceptible. Moreover, prolonged immobility due to injury, surgery, or other health issues can trigger the onset of frozen shoulder. It often develops gradually, typically going through three stages: freezing, frozen, and thawing.
Symptoms to Watch For
The primary symptom of frozen shoulder is persistent pain in the shoulder, which can radiate down the arm. As the condition progresses, the shoulder becomes stiff, making it difficult to perform everyday tasks like reaching for objects or lifting items above shoulder height. Patients may also experience discomfort at night, which can lead to sleep disturbances. Recognizing these symptoms early is crucial for timely intervention and effective treatment.






Recent Comments