Knee and back pain are among the most common reasons people seek orthopedic care. Left untreated, these conditions can significantly affect mobility, daily activities, and overall quality of life. If you are experiencing persistent discomfort, swelling, or limited movement, consulting an expert orthopedic surgeon can make a major difference.
At Orthoone Orthopedics, Bhubaneswar, Dr. Dibya Singha provides advanced orthopedic treatments for knee, back, joint, and spine conditions, helping patients regain mobility and live pain-free lives.
Common Causes of Knee and Back Pain
Understanding the cause of pain is crucial for effective treatment. Some common causes include:
- Knee Pain: Osteoarthritis, ligament injuries (ACL/PCL), meniscus tears, sports injuries, post-trauma conditions.
- Back Pain: Slip disc, spinal stenosis, chronic muscle strain, herniated discs, or degenerative spinal conditions.
- Joint and Muscle Strain: Overuse, improper posture, or sudden injuries.
Why Early Consultation Matters
Delaying orthopedic care can lead to worsening conditions. Early consultation allows:
- Accurate diagnosis through X-rays, MRI, and physical examination
- Personalized treatment plans tailored to your condition
- Minimally invasive interventions before complications arise
- Better long-term outcomes and faster recovery
Advanced Treatments at Orthoone Orthopedics
Orthoone Orthopedics offers a wide range of state-of-the-art treatments, including:
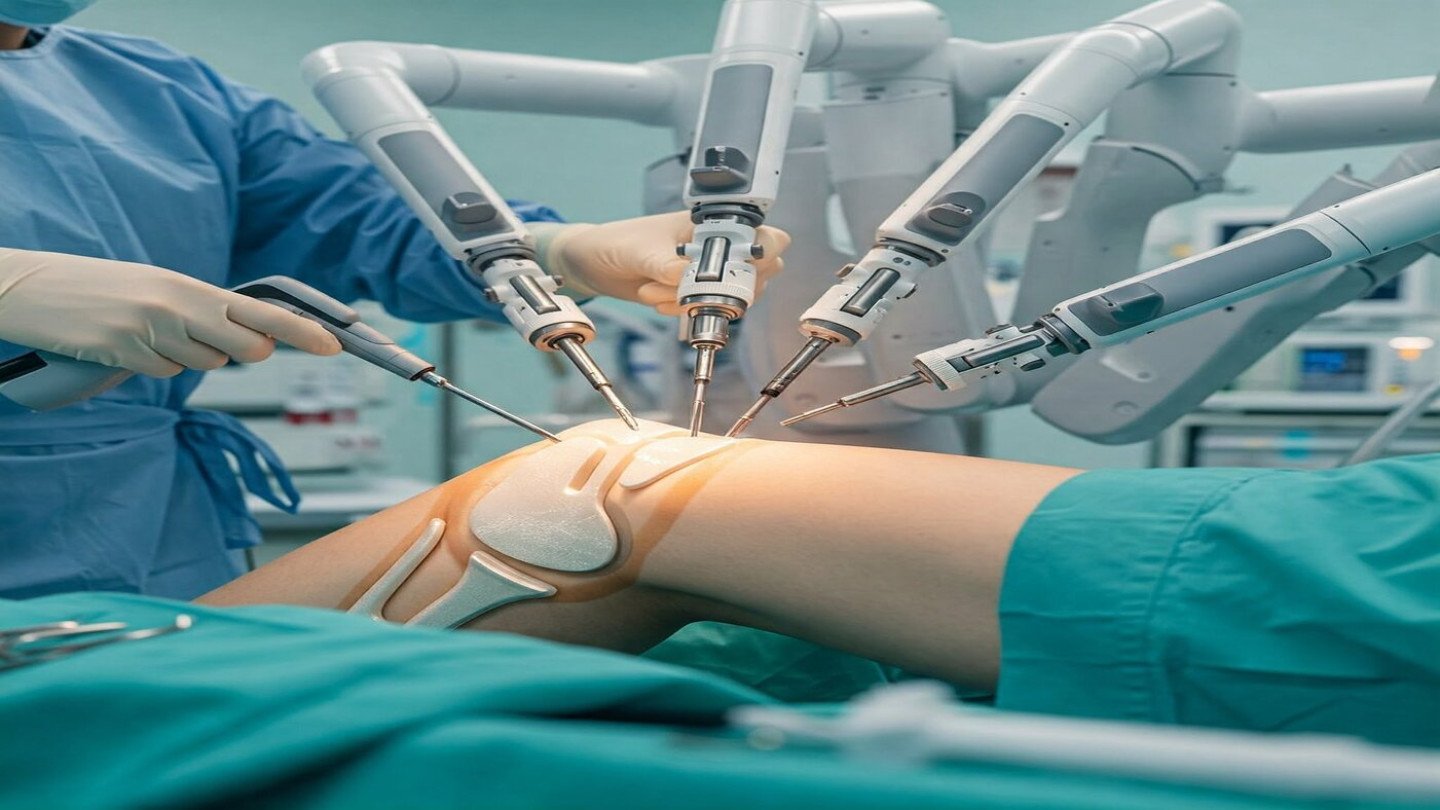
- Robotic Knee Replacement Surgery – precision alignment, faster recovery
- Arthroscopy (Knee & Shoulder) – minimally invasive surgery for ligament and cartilage injuries
- Spine Surgery – slip disc, nerve compression, degenerative spine disorders
- Joint Replacement (Hip, Knee, Shoulder) – pain relief and improved mobility
- Trauma & Complex Trauma Care – fractures, injuries, and limb reconstruction
All treatments are conducted with modern technology and a focus on patient safety and comfort.
Meet Dr. Dibya Singha
Dr. Dibya Singha, Founder & Director of Orthoone Orthopedics, is a highly experienced orthopedic surgeon with over 3,000–5,000 successful surgeries. He combines expertise with compassionate care, ensuring patients are well-informed and confident in their treatment decisions.
Dr. Dibya is a Consultant Orthopedic Surgeon at Utkal Institute of Medical Sciences, providing both advanced surgical care and ethical guidance for patients.
Take Action: Don’t Let Pain Limit Your Life
If knee or back pain is affecting your daily routine, consult Dr. Dibya Singha today. Early intervention can prevent further damage, relieve pain, and restore mobility.
Contact Orthoone Orthopedics
Address: Ortho One Orthopedics
Besides SBI ATM, Back side of Bus Stop
Acharya Vihar Square, Acharya Vihar, Bhubaneswar, Odisha
Phone: +91 94395 37777
Email: drdibyasinghadas@gmail.com
Consultant: Dr. Dibya Singha



Recent Comments